Small Strongyles, also called cyathostomins (or cyathostomes) and small red-worms, are  parasitic gastrointestinal roundworms that affect horses and other equids (donkeys, mules, etc.) worldwide.
parasitic gastrointestinal roundworms that affect horses and other equids (donkeys, mules, etc.) worldwide.
They are among the most harmful worms of horses.
Worldwide there are about 50 species belonging to several genera, with variable prevalence and incidence in the different regions, but not all species are found everywhere.
The most prominent genera are:
- Caballonema spp.
- Coronocyclus spp.
- Craterostomum spp.
- Cyathostomum (=Trichonema) spp.
- Cylicocyclus spp.
- Cylicostephanus (=Trichonema) spp.
- Cylicodontophorus spp
- Gyalocephalus spp.
- Oesophagodontus spp.
- Parapoteriostomum spp.
- Petrovinema spp.
- Poteriostomum spp.
- Tridontophorus spp.
Several surveys in different countries found between 70% and 100% of the horses being infected with these worms. Mixed infections are the rule also with Large Strongyles, with a regional species-specific prevalence. In Europe Cyathostomum catinatum, Cylicostephanus longibursatus and Cylicocyclus nassatus are particularly prevalent. Other common species are Cyathostomum insigne, Cylicostephanus minutus, and Cylicostephanus calicatus. The number of worms in infected animals varies a lot. Immature larvae may be found on infected horses by the thousands.
In the last decades intensive anthelmintic usage has led to a lower frequency of Large Strongyle infections in many places, whereas infections with these Small Strongyles (Cyathostomins) has increased. This seems to be related to the fact that in most places Small Strongyles have become resistant to many anthelmintics, whereas the Large Strongyles have not.
These worms do not affect cattle, sheep, goats, pigs, dogs or cats.
The disease caused by cyathostomin worms is called cyathostomosis or cyathostominosis.
Are horses infected with Small Strongyles contagious for humans?
- NO: There is no evidence that these worms can infect humans.
You can find additional information in this site on the general biology of parasitic worms and/or roundworms.
Final location of cyathostomins
Predilection site of adult cyathostomins is the large intestine (cecum, colon). In contrast with the Large Strongyles, larvae of the Small Strongyles do not migrate into organs outside the gastrointestinal duct.
Anatomy of cyathostomins
Tridontophorus worms are the largest among the cyathostomins, the adult females reaching up to 25 mm in length, almost as long as Strongylus vulgaris, the smallest of the Large Strongyles. Otherwise adults of most other Small Strongyle species are between 10 and 20 mm long. They are white to red in color, due to the ingested blood.
As for other roundworms, the body of these worms is covered with a cuticle, which is flexible but rather tough. The worms have a tubular digestive system with two openings. All species have a characteristic well-formed, rather spherical buccal capsule, in some species equipped with basal teeth that help to cut the host's tissues. They feed on blood and tissues of the organs they migrate through. These worms are so-called plug feeders, i.e. they cut out small chunks of the tissue in the organs where they stay or are migrating through.
They also have a nervous system but no excretory organs and no circulatory system, i.e. neither a heart nor blood vessels. Males have a copulatory bursa, usually with two spicules for attaching to the female during copulation. Morphology of the spicules is species-specific, important for species determination.
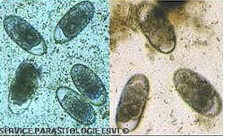
The eggs are ovoid, rather small (~45 x ~105 micrometers) but larger than those of the Large Strongyles. They are thin-shelled and usually contain a morula.
Life cycle of cyathostomins
All cyathostomins have a direct life cycle, i.e. there are no intermediate hosts involved. In contrast with the Large Strongyles larvae of cyathostomins do not migrate out of the intestine towards other organs to later come back, but remain inside the gut during their whole parasitic life cycle inside the host.
Adult females lay eggs in the large intestine of the host that are shed with the feces. A single female worm can produce several thousand eggs daily during several months, with peaks during the summer months in regions with moderate climate. Once in the environment the eggs develop to L3-larvae rather quickly depending on temperature and humidity, within 3 days by warm and moist weather, otherwise within a few weeks.
After the molt to L3-larvae, the skin is not shed, but the larvae remain inside and cannot eat nor continue development until they are ingested by a suited host. This protective membrane protects the larvae to some extent from adverse climatic conditions and increases their chance for survival, which is highly dependent on humidity: dryness causes high larval mortality. By good conditions they may survive for several weeks in the soil. They can even survive through the winter in regions with moderate or cool weather.
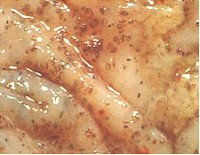
After infective L3-larvae are ingested with contaminated food or water, they hatch out of the protective sheath before reaching the large intestine. There they burrow in to the mucosa of the cecum or colon and become encysted. Up to 90% of the encysted larvae become dormant (or inhibited), i.e. their further development is inhibited. They can remain dormant between 4 months and up to 2 years.
In regions with a cold winter, most larvae ingested during late summer will undergo dormancy until next spring when the environmental conditions become again favorable for larval development, both inside the animals (more food, less stressed animals) and outside (warm and humid climate). Mass emergence of dormant larvae in spring can be extremely harmful for horses, even fatal. The same happens in warm regions during the dry season.
After they leave the cysts, larvae complete development to adult worms in 6 to 12 weeks, mate and the females start laying eggs. The prepatent period (time between infection and first eggs shed) is 5 to 18 weeks, indicating that more than one generation can follow during a normal season. But if larvae become inhibited it can be much longer.
Harm caused by cyathostomins, symptoms and diagnosis
Small strongyles have become the most harmful and prevalent parasitic worms in horses in many regions. This is related to the fact that many small strongyles have developed resistance to the most common anthelmintics used for their control in the last decades.
Little is known about the pathogenicity of the different species, because mixed infections are the rule.
All species and stages feed on the tissues of the intestinal mucosa, also those larvae that do not encyst. This can cause diarrhea, weight loss, weakening and lethargy. Larvae penetrating the gut wall are particularly harmful. Once encysted, each cyst disturbs the normal functioning of the gut around it, and since thousands of cysts may develop, the global physiology of the large intestine can be substantially impaired, severely disturbing nutrition.
However, the heaviest damage is caused by mass emergence of dormant larvae in late winter or early spring, which can severely damage the wall of the intestine and is known as "larval cyathostominosis". In such cases the gut will suffer from bleeding, ulcers and necrosis (death tissue) that are characterized by heavy chronic diarrhea, fever, swelling (edema), often colic and up to 50% fatalities.
Foals and young horses are particularly at risk of suffering severe damage, but adult horses can also suffer the disease all around the year.
Horses that have been exposed to Small Strongyle infections may acquire resistance, but rather slowly and often not to the point that they become immune to it. Damage may be less dramatic but still causing clinical signs and by remaining infected they will continue shedding eggs that contaminate the pastures. This is particularly significant for the transmission of worms to young foals through infective larvae produced by their mother mares in shared pastures.
Diagnosis. Detection of typical eggs or immature larvae in the feces allows to conclude on cyathostomin infection, but usually not sufficient for species determination. This requires coproculture to isolate the larvae, which is rather laborious. Research to develop accurate and easy-to-use diagnostic tools have not yet resulted in a commercially available test kit. Clinical signs are not specific and can be caused by other conditions.
Prevention and control of cyathostomin infections
Non-chemical prevention
An important measure to reduce the risk of infection is to avoid overstocking, because if too many animals share the same pastures, horses will rather eat grass contaminated by manure, which increases the risk of ingesting infecting larvae. Ideally each animal should be allocated 2 to 3 acres (0.8 to 1.2 hectares) of land.
Where practicable, consistent manure removal strongly contributes to decrease pasture infestation with infective larvae and thus reduces the risk that a grazing animal becomes infected.
If feasible, too humid pastures should be drained: the dryer the pastures, the lower the survival of infective larvae and the lower the risk of infection for the horses. Frequent manure removal is also recommended and pastures should not be fertilized with fresh manure.
Water tanks should regularly be cleaned and grazing close to them must be avoided: being wet and frequently visited they are likely to be highly contaminated with infective larvae.
To prevent infestations indoors, stable hygiene is crucial. They must be regularly cleaned, manure has to be removed daily and the bedding must be changed regularly. Humidity has to be kept as low as possible, e.g. with adequate ventilation.
Alternate grazing with livestock (cattle, sheep) that are not susceptible to cyathostomin infection may be considered as well, but livestock can carry other parasites that affect horses as well.
Horses coming into a farm must be always checked for pre-existing infections (e.g. through adequate fecal examination) or treated with a broad-spectrum anthelmintic BEFORE they are allowed to share pastures and premises with other horses. In case of doubt quarantine measures must be considered.
Other preventative measures for gastrointestinal roundworms are explained in a specific article in this site (click here.
So far no true vaccine is available against the small strongyles of horses. To learn more about vaccines against parasites of livestock and pets click here.
Biological control of cyathostomins (i.e. using its natural enemies) is so far not feasible. Learn more about biological control of worms.
You may be interested in an article in this site on medicinal plants against external and internal parasites.
Chemical control
Three major classes of anthelmintics are effective against cyathostomin adult worms and larvae in the gut:
- Benzimidazoles (febantel, fenbendazole, mebendazole, oxibendazole, etc), broad-spectrum anthelmintics effective against cyathostomins and other parasitic roundworms. To control inhibited larvae twice the normal dose is required.
- Macrocyclic lactones (mainly ivermectin, moxidectin), broad-spectrum endectocides effective both against numerous roundworms and several external parasites as well. At the usual therapeutic dose moxidectin is effective against all development stages, including larvae encysted in the intestinal mucosa. Ivermectin controls all development stages as well, but not those encysted in the intestinal wall. Moxidectin provides also the longest protection period against re-infestation.
- Tetrahydropyrimidines (e.g. morantel, pyrantel) are also effective against susceptible adult worms but do not control inhibited larvae and they have a narrow spectrum of activity when compared with benzimidazoles and macrocyclic lactones.
Several commercial products contain mixtures of two or even more active ingredients of different chemical classes. This is sometimes done to extend the spectrum of activity (e.g. to ensure efficacy against roundworms and tapeworms) or to increase the chance that at least one active ingredient is effective against gastrointestinal worms that have become resistant, or to delay resistance development by those worms that are still susceptible.
Depending on the country most of these anthelmintics are available for oral administration as pastes, gels or other formulations for oral administration (e.g. tablets, drenches, feed additives). Very few are available as injectables. Many horse owners complain about the high prices of ivermectin formulations (mostly pastes or gels) for horses when compared with injectables for cattle and other livestock. The reason why ivermectin (or other macrocyclic lactone) injectables are usually not used on horses is apparently that shortly after introduction, it was noticed that horses were more prone to develop severe clostridial infections at the injection site (due to contamination of the needles) and other undesired side effects than cattle or sheep. In addition, the pharmacokinetic behavior of ivermectin on horses is different than in ruminants. For these reasons oral pastes (or gels) were developed for horses that do not show such side effects.
Most wormers containing benzimidazoles (e.g. febantel, fenbendazole, oxibendazole, mebendazole, etc), tetrahydropyrimidines (e.g. morantel, pyrantel) and other classic anthelmintics kill the worms shortly after treatment and are quickly metabolized and/or excreted within a few hours or days. This means that they have a short residual effect, or no residual effect at all. As a consequence treated animals are cured from worms but do not remain protected against new infections. To ensure that they remain worm-free the animals have to be dewormed periodically, depending on the local epidemiological, ecological and climatic conditions. Exceptions to this are macrocyclic lactones (e.g. ivermectin, moxidectin) that are stored in the body fat and progressively released. They offer several weeks protection against re-infestation, depending on the dosage, the delivery form and the specific parasite. Against cyathostomins moxidectin achieves the longest protection, which allows less frequent treatments.
Strategic treatment regimes to reduce pasture contamination with infective larvae are a must to reduce the harmful effects of cyathostomin infections. They must be set up based on local climatic and ecological conditions, on farm management practices, on the approved products that vary from country to country, and on the resistance situation in each farm. Ask your veterinarian for specific local recommendations.
Resistance of cyathostomins to anthelmintics
After decades of intensive use of active ingredients from a limited number of chemical classes, resistance of small strongyles to anthelmintics is widespread and can be rather high, particularly to benzimidazoles (e.g. febantel, fenbendazole, oxibendazole, mebendazole, etc). In a survey from 2009 resistance to benzimidazoles was confirmed in >80% of the investigated yards in UK and Germany. It is known to be also frequent in the US, Australia and in many other countries, including Latin America.
Resistance to tetrahydropyrimidines (e.g. morantel, pyrantel) has also been reported in Europe and the USA, but not as high and frequent as to benzimidazoles, and often a useful degree of efficacy can be still achieved.
Tolerance to macrocyclic lactones (e.g. ivermectin, moxidectin), manifested as a low but significant worm egg output after treatment (determined after fecal egg counts) is not yet widespread, but has been already reported in Europe (e.g. in the UK, Germany, Italy), the USA, and Brazil.
This means that if an anthelmintic fails to achieve the expected efficacy against these worms, chance is significant that it is due to resistance and not to incorrect use, which is the most frequent cause of product failure. Or the product used was not adequate for the control of small strongyles.
Resistance is likely to spread and strengthen worldwide unless serious efforts are taken to reduce the selective pressure exerted on the worms by the intense use of anthelmintics on horses. This can be achieved e.g. through periodically alternating the chemical class of the anthelmintics used (so-called rotation), but also increasing the use of non-chemical control measures such as those previously mentioned (e.g. fecal removal on pastures). This is urgent because there are no indications that new compounds without cross-resistance to those already available may be discovered and developed for horses soon. No such new compounds have been introduced for horses since the discovery of ivermectin in the early 1980s.
Learn more about parasite resistance and how it develops.
|
Ask your veterinary doctor! If available, follow more specific national or regional recommendations for cyathostomin control. |